MYELOPROLIFERATIVE DISORDERS (MPDS)
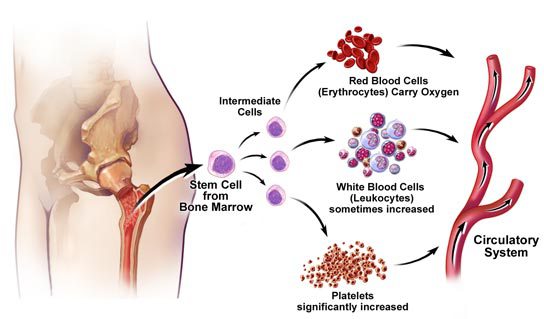
- Chronic myeloproliferative neoplasm or diseases in which the Bone marrow abnormally makes too many red blood cells, platelets, or certain white blood cells.
- Essential thrombocythemia (ET), polycythemia vera (PV), and myelofibrosis (MF) are 3 Philadelphia chromosome−negative
- The used of immunotherapies like Ruxolitinib/Imatinib mesylate, a tyrosine kinase inhibitor used to treat certain types of myelofibrosis.
- Overactive JAK Pathway Signaling Is a Key Mechanism of Disease in MPNs
When the progression of immature blood cells elements in the bone marrow do not progress to mature healthy blood cells, the term myelodysplastic syndrome, myelodysplastic/myeloproliferative neoplasms are used when the disorder has features of both myelodysplastic syndromes and myeloproliferative neoplasms.
Biologically, certain types of myeloproliferative neoplasms and myelodysplastic syndromes may change their cytology and molecular characteristic and transformed into a type of blood cancer called acute leukemia.
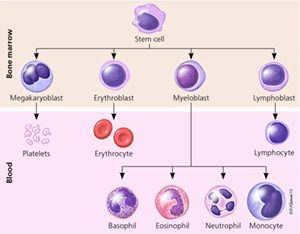
Bone marrow stem cells have the ability to transform into myeloid stem cells or lymphoid stem cells. The lymphoid stem cells become lymphocytes, a type of white blood cells. Myeloid stem cell becomes one of the 3 types of mature blood cells:
- Red blood cells that carry oxygen and other substances to all tissues of the body.
- White blood cells that have the function of fighting infection, cells, and diseases.
- Platelets that are the blood clotting forming cells and are effective in stopping the bleeding.
What are the symptoms of Leukopenia?
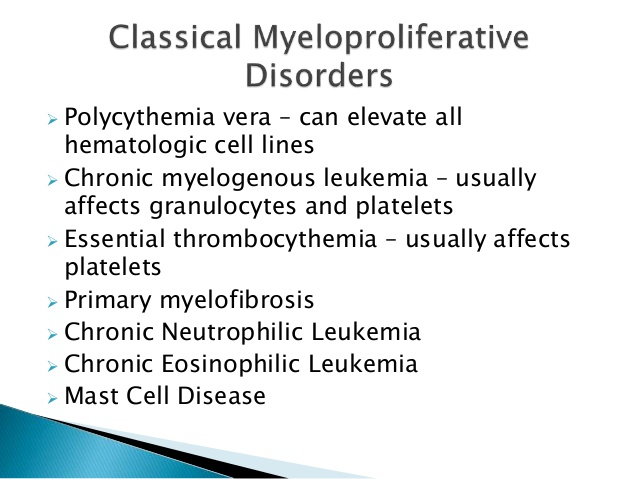
The transforming ability of the blood stem cells, give them the ability to become one or more types of blood cell and give rise to the six chronic myeloproliferative neoplasms recognize today, which include:
- Chronic myelogenous leukemia.
- Polycythemia vera.
- Primary myelofibrosis (also called chronic idiopathic myelofibrosis).
- Essential thrombocythemia.
- Chronic neutrophilic leukemia.
- Chronic eosinophilic leukemia.
Molecular findings in Myeloproliferative Disorder
Myeloproliferative neoplasms (MPNs), which are also known as myeloproliferative disorders (MPDs), share molecular and cellular characteristics but differ in phenotype and clinical presentation. Essential thrombocythemia (ET), polycythemia vera (PV), and myelofibrosis (MF) are 3 Philadelphia chromosome−negative [Ph(−)] MPNs characterized by increased clonal proliferation of myeloid cells. In these myeloproliferative disorders, unregulated proliferation may occur in one or more myeloid cell lines, including erythrocytes, platelets, and granulocytes.
Overactive JAK Pathway Signaling Is a Key Mechanism of Disease in MPNs
Well-regulated JAK signaling is essential for cell production, cell proliferation, and immune function. Intracellular regulators, such as suppressor of cytokine signaling (SOCS), help regulate JAK signaling.
Cytokines bind to receptors and activate JAKs. JAKs activate signal transducers and activators of transcriptions (STATs), which dimerize and enter the nucleus. Inside the nucleus, the STATs bind to DNA, stimulating the expression of genes related to cell survival, differentiation, and proliferation.
Factors that impact JAK signaling:
- JAK2 mutations
- MPL mutations
- Excess cytokines
- Increased JAK1 signaling
- Impaired negative signaling mechanisms (eg, those involving SOCS)
- JAK = Janus-associated kinase
- MPL = myeloproliferative leukemia virus oncogene
- STAT = signal transducer and activator of transcription
How is a chronic myeloproliferative neoplasm diagnosed?
Like most blood disorders, a thorough physical examination and medical history are essential.
–Complete blood cell count (CBC) with differential: A sample of blood is drawn and analyzed for the number of red blood cells and platelets, number and type of white blood cells, amount of hemoglobin and the red blood cells, and the portion of the blood sample made up of red blood cells. In addition, from this CBC a peripheral blood smear is made to study the morphology of the red blood cells, the number, and types of white blood cells, and normal platelets, on addition; check for the presence of blast cells.
–Blood chemistry studies: In this procedure blood sample is taken to measure the quantity of certain substances released into the blood by organs and tissues in the body.
–Bone marrow aspiration and biopsy: in this procedure, a hollow needle is inserted In the hip or breast bone, and bone marrow, blood and a small piece of bone is removed. These are examined by a pathologist under a microscope to look for abnormal cells,
The same sample it is normally used for flow cytometry, fluorescent in situ hybridization, cytogenetics, and gene mutation test; the mutations currently tests are Jak 2, MPL, and CALR. A Jak-2 gene mutation is often found in patients with polycythemia vera, essential thrombocythemia, or primary myelofibrosis. MPL or CALR gene mutations are found in patients with essential thrombocythemia or primary myelofibrosis.
Chronic Myelogenous Leukemia
Chronic myelogenous leukemia, CML is a disease in which too many white blood cells are made in the bone marrow. See review of CML
Polycythemia Vera
Polycythemia vera is disorder in which too many red blood cells are produced in the bone marrow. There is an increase in red blood cell mass along with an increased blood volumes viscosity. For Polycythemia Vera the age of diagnosis is around 60 years old. A male predominance ranges from 1: 1.6 to 2.2. General frequency is 2-3/100,000 population.
Participants of nuclear weapon test are at higher risk of developing the disorder. The medial survival is approximately 12-13 years.
Many other symptoms include headaches and feeling of fullness below the ribs on the left side, this is due to the enlargement of the spleen.
Polycythemia vera is diagnosed by special blood tests, including erythropoietin test and the presence of gene mutation abnormalities. A Jak-2 gene mutation is often found in patients with polycythemia vera,
Additional symptoms include:
- -Feeling of pressure fullness below the ribs on the left side.
- –Headaches.
- –Normal vision seeing dark blind spots that come and go.
- –Itching all over the body, especially after being in warm or hot water.
- –Weakness.
- –Dizziness.
- –Weight loss for no apparent reason.
Primary Myelofibrosis
When fibers and abnormal cells build up in the bone marrow, the condition is called primary myelofibrosis. Myelofibrosis is normally diagnosed around 50–60 years old.
Symptoms of primary myelofibrosis include pain below the ribs on the left side and feeling very tired. Certain factors affect prognosis and treatment options for primary myelofibrosis.
Symptoms of primary myelofibrosis include:
–Pain below the ribs on the left side and feeling very tired.
–Feeling full sooner than normal when eating.
–Feeling very tired.
–Shortness of breath.
–Easy bruising or bleeding.
–Red, flat, pinpoint spots on the skin that are caused by bleeding and refer as petechia.
–Night sweats.
–Fever.
-Weight loss
Prognostic factors and treatment options for primary myelofibrosis include:
Age of patient.
Number of abnormal red blood cells and white blood cells.
The number of blast in the blood.
The presence of certain changes in the chromosomes.
Signs of fever, night sweats, or weight loss.
Essential Thrombocythemia
When too many platelets are made in the bone marrow, the condition is called essential thrombocythemia. Essential thrombocythemia is a very rare disorder affecting 1.5 per 100,000 population. The age of diagnosis is around 60. The female to male ratio is 1.6: 1.
Some of the associated risk factors include the long-term use of direct dark hair dyes, living in a tuff house, and working as an electrician.
It is characterized by proliferation of megakaryocytes causing a marked increase in circulating platelets. These patients may have no signs of symptoms. But the ones that have some symptoms normally complain of:
Headaches.
Burning or tingling in the hands or feet.
Redness or warmth of the hands and feet.
Vision or hearing problems.
Blood clots
Increased bleeding. This can cause serious health problems such as stroke or heart attacks.
Chronic Neutrophilic Leukemia
Chronic neutrophilic leukemia is a disease in which to many blood stem cells, become a type of white blood cells call neutrophils–infection/biting blood cells that destroyed dead cells and bacteria. Common signs are enlarged spleen and liver.
Chronic Eosinophilic Leukemia
Chronic eosinophilic leukemia is cancer in which too many white blood cells (eosinophils) are made in the bone marrow.
Eosinophils are white blood cells that react to and help fight infections caused by certain parasites; also, react to allergens. In chronic eosinophilic leukemia, there are too many eosinophils in the blood, bone marrow, and other tissues. Chronic eosinophilic leukemia may stay the same for many years or it may progress quickly to acute leukemia.
Some of the signs and symptoms associated with chronic eosinophilic leukemia are the following:
- Fever.
- Feeling very tired.
- Cough.
- Swelling of the skin around the eyes and lips, and throat, or on the hands and feet.
- Muscle pain.
- Itching.
- Diarrhea.
What is the treatment for chronic myeloproliferative disorders?
There is no single treatment for chronic myeloproliferative disorders. During the treatment process, it is important to know the type in order to determine the most effective approach.
These are the standard treatment plans which are used:
- Watchful waiting: Closely observation of the patient
- Phlebotomy: During this procedure, approximately 500 to 1000cc of blood is taken from the vein.
- Platelet apheresis: The removal of platelets with a special machine
Transfusion therapy: giving red blood cells, white blood cells or platelets to replace blood cells destroyed by disease or Cancer treatment.
Chemotherapy: Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells either by killing the cells are by stopping them from dividing
- Radiation therapy: uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. There are two types of radiation therapy
- Other drug therapy: the used of prednisone and danazol
- Surgery: Splenectomy or removal of the spleen
- Biologic therapy: consist of the used of interferon alfa and pegylated interferon alpha are biologic agents commonly used to treat some chronic myeloproliferative neoplasms. Also, the use of Thalidomide, lenalidomide, or pomalidomide. Erythropoietic growth factors are also used.
- Targeted therapy: The used of immunotherapies like Ruxolitinib/Imatinib mesylate, a tyrosine kinase inhibitor used to treat certain types of myelofibrosis.
- High-dose chemotherapy with stem cell transplant: High-dose chemotherapy with stem cell transplant is a method of giving high doses of chemotherapy and replacing blood-forming cells destroyed by the cancer treatment. Stem cells (immature blood cells) are removed from the blood or bone marrow of the patient or a donor and are frozen and stored. After the chemotherapy is completed, the stored stem cells are thawed and given back to the patient through an infusion. These reinfused stem cells grow into (and restore) the body’s blood cells.
The information in this document does not replace a medical consultation. It is for personal guidance use only. We recommend that patients ask their doctors about what tests or types of treatments are needed for their type and stage of the disease.
Sources:
- American Cancer Society
- The National Cancer Institute
- National Comprehensive Cancer Network
- American Academy of Gastroenterology
- National Institute of Health
- MD Anderson Cancer Center
- Memorial Sloan Kettering Cancer Center
- American Academy of Hematology